|
Percutaneous nephrolithotomy using
ureteroscope and pneumatic intracorporeal
lithotripsy in the management of pediatric
renal calculi
Xiang Yan, Xiao-Gong Li, Wei-Dong Gan, Hong-Qian Guo
Nanjing, China¡¡
Author Affiliations: Department of Urology, Affiliated Drum Tower Hospital, Nanjing University, Nanjing 210008, China (Yan X, Li XG, Gan WD, Guo HQ)
Corresponding Author: Hong-Qian Guo, MD, Department of Urology, Affiliated Drum Tower Hospital, Nanjing University, Nanjing 210008, China (Tel: 86-25-83105107; Fax: 86-25-83105107; Email: enshine@163.com)
Background: Percutaneous nephrolithotomy (PCNL) is widely performed in the treatment of kidney stones in children. The main risk of this therapy is hemorrhage that requires blood transfusion associated with an increased risk of kidney loss. This study was undertaken to assess the safety and efficacy of PCNL using ureteroscope and pneumatic intracorporeal lithotripsy in the treatment of pediatric renal calculi.
Methods: We studied 22 kidneys of 15 patients under 14 years who underwent PCNL in our hospital. The average age of these patients was 9.2 years (range 5-14 years). In 7 bilateral and 8 unilateral cases of 5 staghorn calculi, the average stone burden was 2.04 (0.9-4.5) cm. PCNL was performed with an X-ray-guided peripheral puncture. With a minimal dilatation of the urinary tract with ureteroscope and pneumatic intracorporeal lithotripsy, a staged approach was used for bilateral cases.
Results: Complete stone clearance was achieved in 20 of the 22 kidneys, giving an overall clearance rate of 91%. Mild fever (<39ºC, <2 days) was seen in 14 patients, whereas serious pyrexia was seen in 1. The decrease in the level of hemoglobin averaged 1.6 g/dl, but none of the patients required blood transfusion.
Conclusions: PCNL is a better treatment of choice for pediatric stone disease refractory to extracorporeal shock wave lithotripsy. To treat pediatric urolithiasis with PCNL using ureteroscope and pneumatic intracorporeal lithotripsy is safe and effective.
Key words: percutaneous nephrolithotomy; ureteroscope; pneumatic intracorporeal lithotripsy; children
World J Pediatr 2007;3(2):146-149
Introduction
Although extracorporeal shock-wave lithotripsy (ESWL) may be used to remove most pediatric renal calculi, percutaneous nephrolithotomy (PCNL) is increasingly important for the patients who failed from shock-wave lithotripsy treatment.[1,2] At present, instruments of adult PCNL are used in the treatment of most children with renal stone.[3,4] PCNL using ureteroscopy and pneumatic intracorporeal lithotripsy may be more safe and effective in children than conventional percutaneous nephrolithotomy in adults.[5,6] During the 2-year period from July 2002 to August 2004, PCNL using ureteroscope and pneumatic intracorporeal lithotripsy was performed in 15 consecutive pediatric patients in our hospital. In this study, we assessed the safety and efficacy of this therapy in the removal of pyelocaliceal stones in these children.
Methods
We studied 22 kidneys of 15 patients under 14 years of age who had undergone PCNL using ureteroscope and pneumatic intracorporeal lithotripsy in our hospital. In this series, 9 were boys and 6 girls, aged from 5 to 14 years (9.2 ¡À 2.7 years), including 7 bilateral and 8 unilateral cases; 5 of the 15 patients had staghorn calculi. Their average stone burden was 2.04 cm (range 0.9-4.5 cm). Ten patients developed acute flank pain, 3 patients had gross hematuria, and 3 patients had urinary tract infection. Two of the 15 patients were diagnosed by ultrasonography incidently. Preoperative examinations included urine culture and sensitivity tests, ultrasonography, plain radiography, intravenous urography, and computed tomography. ESWL was performed repeatedly in 4 patients, but the efficacy of lithotripsy and stone removal was unsatisfactory.
Percutaneous nephrolithotomy using ureteroscope and pneumatic intracorporeal lithotripsy was performed in all patients after general anesthesia. The appropriate calyx was punctured with a 22-gauge Chiba needle (Cook, Bloomington, IL, USA) under real-time X-ray guidance. It was commonly done through a lower pole calyx or the posterior-inferior aspect of the renal stones. Nephrostomy tract dilation was performed with serial dilators (Cook, Bloomington, IL, USA) through the guide wire (Fig. 1A-F). The diameter of tract was determined according to the size of the calyx and the age of the patient.
Fig. 1. Nephrostomy tract dilation with serial dilators through the guide wire. A: the patient in prone position; B-C: puncture under real-time X-ray guidance; D: peel-away sheath for percutaneous access; E-F: tracts dilated using serial dilators; G-H: ureteroscope (Wolf) and pneumatic intracorporeal lithotripsy; I: a nephrostomy tube placed to drain the kidney.
The 12-Fr or 14-Fr peel-away sheath was used in 12 kidneys, in which the collecting system was not distended. The 16-Fr peel-away sheath was used in 7 kidneys, in which the collecting system was distended and the stone was larger. The 18-Fr peel-away sheath was used in 3 kidneys, in which the collecting system was distended obviously and the stones were much larger. In 10 kidneys of patients under 8 years, the 12-Fr or 14-Fr peel-away sheath was used. While in 12 kidneys of patients over 8 years, the 16-Fr or 18-Fr peel-away sheath was used. Single access tract was established in 14 kidneys. Dual access tracts were established in 8 kidneys in consideration of the stone location in the calyx, calyx direction and calyx neck. 26 access tracts were formed via the middle posterior calyx, 2 access tracts were established via the lower pole calyx. The first tracts were dilated to 12Fr-18Fr, and all the second tracts were dilated to 12-Fr. A 9.8-Fr rigid ureteroscope (Wolf) and a pneumatic lithoclast was used in all cases (Fig. 1G-H). Small fragmented stones were extracted by suction and grasping forceps. At the end of the procedure, a nephrostomy tube was placed to drain the kidney (Fig. 1I).
After tubes of PCNL nephrostomy were clamped for 2-3 hours, a plain abdominal film was taken to evaluate residual stones. The patient was defined as stone-free if there was no residual fragments on a plain abdominal X-ray. The tubes were removed after 4-5 days when the urine was clear.
Results
In most of patients, nephrostomy tract dilation and stone extraction were performed successfully (Fig. 2). The operation was discontinued because of a large amount of blood loss during the dilation process (in 2 patients) and in the process of fragmenting stones (in 3 patients), but the second repeated operations were all successful. In 2 patients with pyemia, a nephrostomy tube was placed in the renal pelvis at first, and PCNL was performed after infection was controlled.
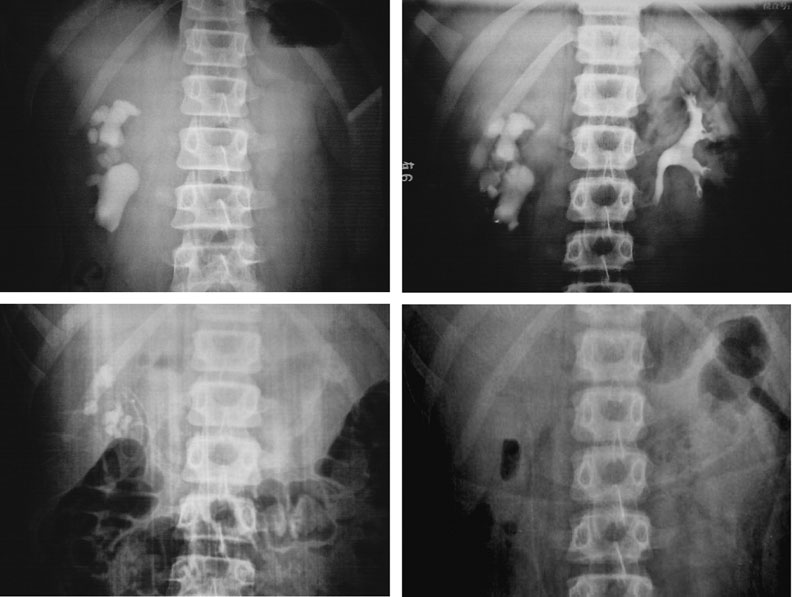
Fig. 2. Nephrostostomy tract dilation and stone extraction. A: plain film (KUB); B: intravenous urography (IVU); C: KUB after the first stage of MPCNL; D: KUB after the secondary stage of MPCNL.
The mean duration of PCNL was 75 minutes (range 45-120 minutes), including the time for general anaesthesia, initial cystoscopy, retrograde catheterization and turning the patient in prone position. Complete clearance was achieved in 20 kidneys (91%) after PCNL monotherapy. Two kidneys were cleared of stones after adjunctive ESWL for residual fragments. Mild fever occurred in 2 (13.3%) of the 15 patients, and subsided spontaneously within two days. The average fall in hemoglobin was 14¡À8 g/L (range 5-27 g/L). None of the patients received blood transfusion. The median length of hospital stay was 5.2 days (range 4-13 days).
The patients were followed up every 6 months for 2 years and yearly thereafter by a urine culture test and ultrasound examination. Three patients were lost to follow-up after the first visit, while 12 patients completed at least 2 years of follow-up. To date, there has been one recurrence of stone, and no other complications occur.
Discussion
Since the advent of PCNL in 1976, the techniques have been greatly improved.[7,8] Many medical centers have used adult-sized nephroscopes in children. But percutaneous stone therapy-related hemorrhage requires a blood transfusion (11%-14%), and an increased risk of kidney loss.[8,9] Therefore, conventional percutaneous nephrolithotomy is not justified as the primary form of urinary stone treatment for smaller lower pole concrements, although it is recommended as an effective method in children.[10-12] Percutaneous nephrolithotomy using ureteroscope and pneumatic intracorporeal lithotripsy in children was introduced to our hospital in 2002. In this study, the stones were removed completely with minimal injury to renal tissue, while retrieving large fragments quickly. The duration of the procedure was 75 minutes. The level of hemoglobin decreased by 14¡À8 g/L on average. None of the patients received blood transfusion. To date, there has been only one recurrence of stone and no other complications occur.
Traditional percutaneous nephrolithotomy uses a 30-Fr nephrostomy sheath for renal access. In order to reduce blood loss and absorption of irrigant, stone extraction may be performed when the established access tracts become mature.[13] The recent development of smaller sheaths suggests that percutaneous nephros-tomy tract formation can be performed with minimal injury to the involved renal parenchyma, thereby reducing the procedure-related morbidity.[14-16] We used ureteroscope and pneumatic intracorporeal lithotripsy in pediatric patients. The operating tract was small (12F-18F), therefore only 2 operations were discontinued because of greater blood loss in the process of dilatation, but the second operations were successful.
During PCNL, the common mistake especially for staghorns in children is overdoing through a single tract, even when another tract is needed.[3] Torquing a rigid ureteroscope against the pelvicaliceal system to get to an inaccessible calix is the most important cause of bleeding during PCNL and is largely responsible for the increased rates of transfusion and extravasation.[17,18] We believe that judiciously making multiple tracts does not significantly increase intraoperative complications and transfusion. Using multiple tracts when necessary avoids the excessive use of torque to gain entry into adjacent calices, which may cause infundibular tear and bleeding.[19,20] In the present series, multiple tracts were used in 8 kidneys. As a result, better and faster clearance of large-volume staghorn calculi was achieved without significant increase in morbidity.
PCNL has a better stone clearance rate and is cost-effective. It is characterized by convalescence compared with other modalities such as ESWL and open surgeries for removal of the stones. In our series, PCNL achieved a complete-clearance rate of 91%, and an overall clearance rate of 100% when it was combined with ESWL. In children with large renal stones (>3 cm), staghorn calculi (complete and partial), complex or multiple calculi, renal insufficiency, recurrent stones, and stones refractory to ESWL, PCNL is considered the treatment of choice. The use of a less traumatic 18-Fr access sheath is effective in children with large renal stones. A prerequisite for stone clearance is the establishment of optimal access to the collecting system of the kidney. Staging the procedure in selecting patients is very important to reduce the caliber of the percutaneous tract in children with non-dilated collecting system.
Funding: None.
Ethical approval: Not needed.
Competing interest: None declared.
Contributors: YX proposed the study and wrote the first draft. LXG analyzed the data. GHQ is the guarantor.
References
1 Fraser M, Joyce AD, Thomas DFM, Eardley I, Clark PB. Minimally invasive treatment of urinary tract calculi in children. BJU Int 1999;84:339-342.
2 Desai MR, Kukreja RA, Patel SH, Bapat SD. Percutaneous nephrolithotomy for complex pediatric renal calculus disease. J Endourol 2004;18:23-27.
3 Aron M, Yadav R, Goel R, Hemal AK, Gupta NP. Percu-taneous nephrolithotomy for complete staghorn calculi in preschool children. J Endourol 2005;19:968-972.
4 Choong S, Whitfield H, Duffy P, Kellett M, Cuckow P, Van't Hoff W, et al. The management of paediatric urolithiasis. BJU Int 2000;86:857-860.
5 Zeng GH, Li X, He ZH, Shan ZC, Yuan J, Chen WZ, et al. Comparision of renal parenchymal injury after mini and standard percutaneous nephrolithotomy. Chin J Exp Surg 2004;21:1551-1552.
6 Lahme S, Bichler KH, Strohmaier WL, Gotz T. Minimally invasive PCNL in patients with renal pelvic and calyceal stones. Eur Urol 2001;40:619-624.
7 Fernstrom I, Johansson B. Percutaneous pyelolithotomy: a new extraction technique. Scand J Urol Nephrol 1976;10:257-259.
8 Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Nephrolithiasis clinical guidelines panel summary report on the management of staghorn calculi. The american urological association nephrolithiasis clinical guidelines panel. J Urol 1994;151:1648-1651.
9 Rodrigues NN, Claro JA, Ferreira U. Is percutaneous monotherapy for staghorn calculus still indicated in the era of extracorporeal shockwave lithotripsy? J Endourol 1994;8: 195-197.
10 Boddy SA, Kellett MJ, Fletcher MS, Ransley PG, Paris AM, Whitfield HN, et al. Extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy in children. J Pediatr Surg 1987;22:223-227.
11 Lahme S. Shockwave lithotripsy and endourological stone treatment in children. Urol Res 2006;34:112-117.
12 Raza A, Turna B, Smith G, Moussa S, Tolley DA. Pediatric urolithiasis: 15 years of local experience with minimally invasive endourological management of pediatric calculi. J Urol 2005;174:682-685.
13 Stapleton FB. Clinical approach to children with urolithiasis. Semin Nephrol 1996;16:389-397.
14 Monga M, Oglevie S. Minipercutaneous nephrolithotomy. J Endourol 2000;14:419-421.
15 Mahmud M, Zaidi Z. Percutaneous nephrolithotomy in children before school age: experience of a Pakistani centre. BJU Int 2004;94:1352-1354.
16 Samad L, Aquil S, Zaidi Z. Paediatric percutaneous nephro-lithotomy: setting new frontiers. BJU Int 2006;97:359-363.
17 Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: prospective study. J Endourol 2004;18:715-722.
18 Boormans JL, Scheepe JR, Verkoelen CF, Verhagen PC. Percutaneous nephrolithotomy for treating renal calculi in children. BJU Int 2005;95:631-634.
19 Manohar T, Ganpule AP, Shrivastav P, Desai M. Percutaneous nephrolithotomy for complex caliceal calculi and staghorn stones in children less than 5 years of age. J Endourol 2006; 20:547-551.
20 Salah MA, Toth C, Khan AM, Holman E. Percutaneous nephrolithotomy in children: experience with 138 cases in a developing country. World J Urol 2004;22:277-280.
Received October 10, 2006; Accepted after revision April 5, 2007
|

