|
Surgical anatomy of the pelvis as a basis for
pull-through procedures in Hirschsprung's
disease
S. Berger, M. Schweizer, P. Schweizer
Bern, Switzerland
Author Affiliations: Department of Surgical Pediatrics, Children's Hospital, Inselspital, University of Bern, Switzerland (Berger S); Department of Anesthesiology, Marien Hospital Stuttgart, Germany (Schweizer M); Depart-ment of Pediatric Surgery, University of T¨¹bingen, Germany (Schweizer P)
Corresponding Author: Steffen Berger, MD, Department of Surgical Pediatrics, Children's Hospital, Inselspital of the University of Berne Freiburgstr, CH-3010 Bern, Switzerland (Tel: 0041-31-632-9274; Fax: 0041-31-632-9292; Email: steffen.berger@insel.ch)
Background: The basis for successful pull-through procedures in patients with Hirschsprung's disease is a detailed knowledge of the anatomy of the pelvis. The currently most utilized pull-through techniques were reviewed with regard to their impact on the anatomy of different regions of the pelvis. The findings were analyzed as to advantages and disadvantages of the respective procedures.
Methods: The anatomy of the pelvis was studied in three children by post mortem examination. The study was approved by the institutional ethics committee.
Results: The study confirmed five anatomical regions of the pelvis of surgical importance which should be considered when planning and performing a pull-through procedure. It could be shown that the fascial coating of the rectum plays an important role in an adequate pull-through procedure.
Conclusions: The type of complications that may be expected and the prognosis of a pull-through procedure is influenced by the given anatomical conditions of the pelvis. Thus, an adequate procedure should respect the anatomical characteristics of the five surgically important anatomical regions of the pelvis.
Key words: Hirschsprung's disease; pull-through operation; pelvic anatomy
World J Pediatr 2007;3(2):134-139
Introduction
The aim of this study is to illustrate and categorize the topographical anatomy of the pelvis from a surgical point of view in order to draw conclu-sions for pull-through procedures. With the help of the anatomy, advantages and disadvantages of the Rehbein-[1], Soave-[2] and Duhamel[3] pull-through techniques as applied in patients with Hirschsprung's disease can be defined. Around the millenium, the classical Rehbein-, Soave-, and Duhamel-procedures were quit in many pediatric surgical facilities in favour of the transanal endorectal pull-through (de la Torre-operation[4]). However, a certain fraction of patients operated with the above mentioned techniques will still require secondary surgery such as a redo pull-through years from now on. Long-term results of the de la Torre-operation which is a modified Soave procedure are still scarce, data on redo-de la Torre-operations after a previous Soave- or de la Torre-operation are not published so far. In respect to a pull-through procedure and especially a redo pull-through, the surgeon must consider different topographical regions of the pelvis. These regions will be presented in this study along with findings from post mortem examinations of children.
Blood supply to the rectum is maintained by three levels of arteries. The single superior rectal artery originates from the inferior mesenteric artery and branches into the upper and middle part of the rectum. It enters the mesosigmoid well above the peritoneal fold. The inferior part of the rectum which is below the peritoneal fold but still above the levator ani is perfused via the A. rectalis media originating from the internal iliac arteries and entering the rectum bilaterally. The A. rectalis media penetrates the hypogastric nerve plexus on its way to the rectal wall. Inferior to the levator ani, the rectum receives blood supply bilaterally from the inferior rectal arteries which come from the internal pudendic artery after passing Alcock's canal. The innervation of the rectum, anus and pelvic floor is complex and still not fully understood. Therefore, only a rough outline of this complex situation is presented in the following. First, autonomic innervation and somatic innervation can be distinguished.
Autonomic innervation is composed of sympathetic (Th 11/12 ¨C L 1/2) and parasympathetic (vagus + S 1-3) influences. In general, sympathetic stimulation decreases while parasympathetic stimulation increases peristalsis and secretion.[5] Predominantly sympathetic fibers from the superior hypogastric plexus projecting through the bilateral fiber bundles of the hypogastric nerve and fibres from the sacral splanchnic nerves contribute to the left and right hypogastric plexus. Parasympathetic fibers constitute the pelvic splanchnic nerves and the pelvic plexus. It was recently shown that the posterior part of the inferior hypogastric plexus (IHP) innervates the superior portion of the rectum while the anterior part of the IHP innervates the inferior part of the rectum.[6] Autonomic innervation is of major importance for unconscious control of the internal sphincter, the inferior hypogastric plexus is located above the pelvic diaphragm at the level of the S 4/5 vertebrae.
The afferent pathways consist of 1) the visceral afferent fibres which accompany both parasympathetic (cell bodies in S 1-4 dorsal root ganglia) and sympathetic efferent fibres (cell bodies in Th 11-L2 dorsal root ganglia) and 2) the somatic fibres (cell bodies in S 1-4 dorsal root ganglia) which accompany the pudendal nerve (pudendic plexus) and direct somatic branches of the sacral plexus. These pathways are of importance for conscious sensory perception and for control of the external sphincter, the pudendic nerve is located below the pelvic diaphragm.
In summary, all the above mentioned neural structures form plexuses in the anorectal environment which are densely connected and interact in a complex manner. Nerve-sparing operative technique is therefore a prerequisite for a successful outcome in anorectal surgery.[6,7] Knowledge of the topographic relation of the respective neural structures to the pelvic connective tissue is of major relevance for performing operations in Hirschsprung's disease and other anorectal malformations.[8] However, this aspect has received little attention in pediatric surgery so far although it is a major issue in other surgical fields such as for resection of rectal carcinoma[9] or prostatic cancer.[10] Furthermore, age-specific differences may have an impact when operating in neonates: anatomic studies in fetuses revealed relatively thick nerves[11] surrounded by little connective tissue while studies in adults showed relatively tiny nerves embedded in thicker connective tissue.[6]
Methods
The topography of the pelvis was studied by post mortem examinations in two still-born term neonates and in a three-year-old female child who died in an accident. The study was approved by the Ethics Committee of the hospital.
From a surgical point of view the pelvis was divided into the following five different regions. Region I: the region of the anterior peritoneal excavation; region II: the region behind the sigmoid colon and the recto-sigmoid junction; region III: the region behind the rectum; region IV: the region in front of the rectum; and region V: the region of the ano-rectal portion below the pelvic floor.
Special attention was given firstly to the arteries of the sigmoid colon, the recto-sigmoidal junction, the rectum and the anorectum, secondly to the nerves of the presacral plexus and the nervus pudendus, thirdly to the fascial coating which covers the rectum and the two lateral wings (also named "ailerons lateraux" or "mesorecta").
The preparation of the structures in question was performed according to the technique of a Duhamel pull-through procedure.
In order to prevent (expensive) staining methods the anatomy was reconstructed by sketches since photographs of the native anatomical structures situated deep inside the pelvis did not represent the anatomy properly. The results hereof were compared with alterations of the pelvic structures in 17 children undergoing a redo pull-through operation.
Results
Region I
The surgical region I corresponds to the anatomy of the anterior peritoneal excavation (Fig. 1). The interrupted line shows the surgical incision of the peritoneum in order to exhibit the region behind the sigmoid colon and the recto-sigmoidal junction. This incision should not be continued to the right side.
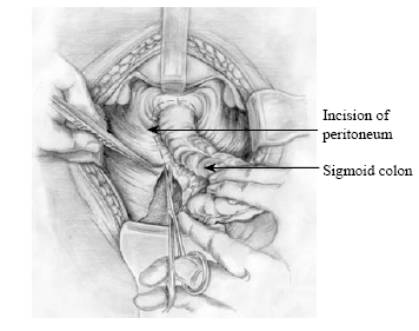 
Fig. 1. Anatomy of surgical region I: anterior peritoneal excavation, peritoneum incised posteriorly on the left side.Fig. 2. Anatomy of surgical region II: Behind the recto-sigmoidal junction, the pelvic floor, the promontory, the aortic bifurcation and the left ureter become visible.
Region II
The surgical region II corresponds to the anatomy behind the sigmoid colon and the recto-sigmoidal junction (Fig. 2). After opening the peritoneum on the left side of the sigmoidal mesentery and across the base of the anterior peritoneal excavation, the sigmoidal mesentery containing branches of the inferior mesenteric artery can be presented. In order to exhibit the region behind the sigmoid colon and the recto-sigmoidal junction the mobilized bowel must be straightened both ventrally and strongly to the right side. Then it can be shown that the sigmoid mesentery is only fixed by loose bundles of mesenchymal adhesions on the retroperitoneal space and on the promontory. After dividing these adhesions by sharp preparation the left ureter can be seen laterally and the bifurcation of the abdominal aorta can be identified medially.
Region III
The surgical region III corresponds to the anatomy behind the rectum (Fig. 3). The rectum is sheated by a thin fascial coating from the beginning at the promontory down to the pelvic floor. The dorsal part of this fascia is named Waldeyer's fascia, the ventral part Denonvillier's fascia. As a rule, this fascial coating can be demonstrated by careful preparation. It continues onto the right and left lateral muscular and mesenchymal wings that fix the rectum on the lateral parts of the pelvis (In surgery of rectal carcinoma these wings are called "mesorecta"). They lead branches of the A. rectalis media, branches of the parasympathetic Nn. splanchnici pelvici, and branches of the sympathetic trunk which supply the rectum. They also contain the plexiform branches of the V. rectalis media.
Region IV
The surgical region IV corresponds to the anatomy in front of the rectum (Fig. 4). This region can only be shown if the mobilized bowel is strongly elevated cranially, straightened ventrally and pushed dorsally to the promontory. Then the upper part of the bladder, the two funiculi, the two spermatocystes, the upper part of the prostate in male patients and the bladder as well as the uterus and the upper part of the vagina in female patients can be shown. The mesenchymal adhesions between the bladder and the upper part of the uterus to the rectum are dense and rigid so that they can only be divided by sharp dissection. In the region of the funiculi and the spermatocystes the adhesions become more loose. They can be divided by careful blunt dissection. The blunt dissection can be continued down to the level of the pelvic floor where the adhesions of the rectum to the dorsal wall of the vagina in females and to the posterior urethra in males again become more tense and thus can only be divided by sharp dissection.
Fig. 3. Anatomy of surgical region III: The view behind the rectum which is covered by Waldeyer's fascia extending laterally to the mesorecta with branches of sympathetic and parasympathetic nerves as well as branches of the A. and V. rectalis media. Fig. 4. Anatomy of surgical region IV: Anteriorly the rectum is covered by Denonvillier's fascia. Mesenchymal adhesions to the bladder and uterus or prostate respectively have to be separated. Further down, adhesions to the dorsal wall of the vagina or to the male urethra have to be exposed and dissected carefully.
Region V
The surgical region V corresponds to the anatomy of the anorectal portion. This region begins inferior to the pelvic floor (Fig. 5). The following structures can be demonstrated in this region: the muscular fibers of the sphincters which surround the ano-rectum, the posterior wall of the vagina in females, the posterior urethra in males, the muscular fibers of the pelvic floor, and the ano-coccygeal ligament. Special attention has to be given to the artery and vena pudenda as well as to the right and left N. pudendus.
Structures that are at special risk with the different operative procedures are listed by region in the Table. An overview of localization of the 5 surgical regions is given in Fig. 6.
Fig. 5. The anatomy of surgical region V. Inferior to the pelvis floor muscles, the pudendic nerve and the pudendic vessels should be respected around the anorectum with its muscular sphincters. Fig. 6. Localization of the 5 surgical regions.
Table. Structures potentially compromised by the different surgical procedures within different surgically important perirectal regions
|
|
Region I |
Region II |
Region III |
Region IV |
Region V |
|
Rehbein (Swenson) |
- |
Nn. splanchnici |
Waldeyer's fascia
Lateral wings |
Denonvillier's fascia
IHP spermatocysts |
- |
|
Soave (de la Torre) |
- |
Nn. splanchnici |
- |
- |
- |
|
Duhamel |
- |
Nn. splanchnici |
Waldeyer's fascia |
- |
A.+V. pudenda N.pudendus |
Discussion
The purpose of this study was to present the anatomy of the pelvis in respect of primary and possible redo pull-through procedures in Hirschsprung's disease. The results suggest that conclusions can be drawn from the anatomy of the five regions not only regarding advantages and disadvantages of the different initial pull-through techniques but also for the development of an adequate redo pull-through procedure. The anatomy demonstrates structures of the five regions that conflict the surgeon in a different manner in the different pull-through procedures. The kind and extent of alterations of these structures depend clearly on the technique that is used to mobilize the rectum for the pull-through procedure. Moreover, the results suggest that both the prognosis and the kind of complications after initial pull-through depend on the alterations of the anatomical structures caused by the pull-through procedure and that these alterations are specific for the type of procedure employed. On the basis of the anatomy, the positive and negative effects of the different pull-through techniques are discussed in the following.
Considerations for primary pull-through procedures
Rehbein procedure
Rehbein[1] himself has emphasized that the success of his procedure depends clearly on the length of the ano-rectal segment that is left in place after resection. This segment must not be more than 3 cm in length. Regarding the anatomy of the pelvis, it is evident that such a resection of the rectum is difficult to achieve because of the anatomic conditions found in regions II and III. The findings in redo operations demonstrate clearly that primary resection often has not guaranteed such a short anorectal segment,[12] probably because of the anatomy of the pelvis or shortcomings in operative technique. It is understandable that performing an end-to-end anastomosis in the very depth of the pelvis may be difficult. The frequency of anastomotic strictures and fistulae developing after Rehbein procedures[13] confirms these surgical difficulties. As in Rehbein's operation the rectum must be mobilized circularly down to the pelvic floor, so the risk to damage the presacral nervous plexus in behind and the vessels, the nerves to the bladder, the funiculi and the spermatocystes in front is rather high. A clear expression of this risk may be that 2 patients of a series of 13 in whom a redo pull-through was indicated suffered from urethrodynia and neuronal bladder dysfunction after initial Rehbein operation.[12] Furthermore, one postmortem examination and 13 redo procedures after initial Rehbein operation demonstrated that the formation of scars surrounding the pulled-through bowel was quite extensive so that a redo pull-through procedure was very difficult. During preparation of the pelvis in these 14 patients the fascial coating of the rectum, especially the Waldeyer's and Denonvillier's fascia as well as the two lateral wings of the rectum could not be identified since they were destroyed by the primary operation.[12] In Swenson's procedure[14] the abdominal preparation is similar to Rehbein's procedure, only the anastomosis is made from the perineal side. It is therefore assumed, although not observed in this study, that in regions I-IV similar findings should be expected after a Swenson's procedure as after a Rehbein operation. In region V, the suture line after a Swenson's procedure may be expected further distal than after a Rehbein procedure.
Soave pull-through procedure
As in Soave pull-through procedures the muscular cuff of the rectum remains and thus needs not to be mobilized from the fascial coat, the structures in the surgical region III in front of the rectum and the presacral nervous plexus behind are not at risk from operative damage. Attention has only to be paid on the Nn. splanchnici in front of the bifurcation of the abdominal aorta. However, if one succeeds to preserve the fascial coating of the rectum, especially Waldeyer's fascia, these nerves are not endangered as well.
The most important complication after Soave pull-through procedures is rigidity and stenosis of the anorectum due to formation of sclerotic scars between the layers of the remaining muscular cuff of the native rectum and the pulled-through bowel. This is probably also true after the de la Torre-operation which is a transanal Soave procedure with regard to the surgical regions I-V.
Duhamel pull-through procedure
In the Duhamel procedure, the anatomy of the surgical region III in front of the rectum and the anatomy of the two lateral wings are left untouched.[12,15] So far the structures in these regions are not at risk. However, in the surgical anatomical region II the nerves in front of the bifurcation of the abdominal aorta and the presacral nervous plexus behind the rectum are endangered. Nevertheless, injuries can be prevented if the posterior wall of the rectum is mobilized to perform a retrorectal, presacral, transanal pull-through procedure precisely in the plane between the dorsal rectal wall and Waldeyer's fascia.[12] This means that the proximal circumference of Waldeyer's fascia needs to be identified exactly. This surgical step is not difficult if the surgeon is well acquainted with the anatomy of the surgical regions II and III.
Considerations for redo pull-through procedures
Problems and handicaps in region V, the region of the ano-rectal portion
In initial surgery of Hirschsprung's disease neither the Rehbein operation nor the Duhamel- or Soave pull-through procedure gives rise to problems because of anatomical conditions in this region. However, problems occur in a redo pull-through procedure if scar formation from the initial pull-through procedure (as found after anastomotic insufficiency or interventions such as sphinctermyotomy) renders the mobilization of the bowel more difficult.
Difficulties in redo procedures after initial Rehbein operation
In one third of patients, myectomy was performed after initial Rehbein procedures. In 4 of a series of 13 patients with an initial Rehein operation other surgical procedures have been performed with the intention to remove strictures of the anastomosis.[12] These surgical measures were consistently followed by severe and extensive formation of scars not only surrounding the ano-rectal portion of the bowel but also afflicting the presacral space.
Difficulties in redo procedures after initial Soave pull-through procedure
Difficulties arise after the experiment to repair rigidity or even stenosis of the anorectal cuff by myectomy or even by a large longitudinal division. In one of two patients with an initial Soave pull-through procedure in a series of 17 children who had undergone a redo pull-through procedure, such a surgical measure caused extensive formation of dense sclerotic scars that occluded the inferior region of the presacral space completely.[12]
Difficulties in redo procedures after initial Duhamel pull-through procedure
As in the initial Duhamel procedure, the posterior wall of the anorectal portion has to be incised transversely in order to perform a transanal pull-through procedure of the colon. After such an incision, hematoma may develop in the muscular space between the coccyx and the dorsal circumference of the anus, giving rise to severe formation of sclerotic scars[16] which may make a redo Duhamel procedure difficult.
Conclusions
The mentioned observations are supported (only) by findings in 17 patients with redo operations and 3 post mortem examinations. So far, the results cannot claim any statistical significance. However, on the basis of the presented surgical anatomy of the pelvis, the observations and remarks are proper for criticism of the different pull-through procedures and are as well useful to define principles for an adequate redo pull-through procedure.
Funding: None.
Ethical approval: Ethical Committee of the Hospital.
Competing interest: None declared.
Contributors: BM and SP proposed the study and wrote the first draft, SM analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. SP is the guarantor.
References
1 Rehbein F. Kinderchirurgische Operationen. Stuttgart: Hippokrates Verlag, 1976: 309-367.
2 Soave F. Hirschsprung's disease: a new surgical technique. Arch Dis Child 1964;39:116.
3 Duhamel B. A new operation for the treatment of Hirschsprung's disease. Arch Dis Child 1960;35:38.
4 De la Torre-Mondragon L, Ortega-Salgado JA. Transanal endorectal pull-through for Hirschsprung's disease. J Pediatr Surg 1998;33:1283-1286.
5 Vodusek D. Anatomy and neurocontrol of the pelvic floor. Digestion 2004;69:87-92.
6 Baader B, Herrmann M. Topography of the pelvic autonomic nervous system and its potential impact on surgical intervention in the pelvis. Clin Anat 2003;16:119-130.
7 Church J, Raudkivi P, Hill G. The surgical anatomy of the rectum¡ªa review with particular relevance to the hazards of rectal mobilisation. Int J Colorectal Dis 1987;2:158-166.
8 Fritsch H, Lienemann A, Brenner E, Ludwikowski B. Clinical anatomy of the pelvic floor. Adv Anat Embryol Cell Biol 2004;175:1-64.
9 Stelzner F. Chirurgie der visceralen Abschlußsysteme. Stuttgart: Thieme Verlag, 1998.
10 Tewari A, Peabody J, Fischer M, Sarle R, Vallancien G, Delmas V, et al. An operative and anatomic study to help in nerve sparing during laparoscopic and robotic radical prostatectomy. Eur Urol 2003;43:444-454.
11 Fritsch H. Topography of the pelvic autonomic nerves in human fetuses between 21-29 weeks of gestation. Anat Embryol 1989;180:57-64.
12 Schweizer P, Beck O, Berger S. Repeat pull-through surgery for complicated Hirschsprung's disease (principles derived from clinical experience). J Pediatr Surg 2007;42:536-543.
13 Holschneider A, Sölylet Y, Ebel K. Dysganglionosen (Morbus Hirschsprung, Neuronale Intestinale Dysplasie). In: Schärli A, eds. Komplikationen in der Kinderchirurgie. Stuttgart New York: Georg Thieme Verlag, 1991: 147-164.
14 Swenson O. New treatment for Hirschsprung's disease. Surgery 1950;28:371.
15 Schweizer P, Flach A. Experience with Duhamel's procedure. In: Holschneider A, eds. Hirschsprung's disease. Stuttgart: Hippocrates Verlag, 1982: 168-174.
16 Schweizer P, Pfeiffer J, Feller A. Langzeitergebnisse nach operativer Korrektur des Megacolon congenitum Hirschsprung mit dem Verfahren nach Duhamel und Rehbein. Z Kinderchir 1980;30:339-343.
Received November 3, 2006; Accepted after revision December 10, 2006
|

