|
Improvement of resuscitation techniques for
neonatal asphyxia
Xiao-Yu Zhu, Qian-Shen Zhang
Shenzhen, China
Author Affiliations: Neonatal Department, South Medical University Affiliated Maternal & Child Health Hospital of Shenzhen, Shenzhen 518028, China (Zhu XY, Zhang QS)
Corresponding Author: Xiao-Yu Zhu, MD, Neonatal Department, South Medical University Affiliated Maternal & Child Health Hospital of Shenzhen, Shenzhen 518028, China (Tel: 86-755-83251469; Fax: 86-755-83230651; Email: zhuhaizxy@tom.com)
Four editions of Guidelines for Neonatal Resuscitation of Asphyxia have been issued in China, and the guidelines have been updated every 10 years since the 1980s to keep up with the international standards.[1-4] Since the 4th edition (2000 edition) of Neonatal Resuscitation and its flow algorithm of the American Academy of Pediatrics has been translated into Chinese,[5] the 4th edition of Chinese Guidelines for Neonatal Resuscitation of Asphyxia has been comprehensively updated in 2005.[6,7] Thereafter, nationwide training in neonatal resuscitation has been carried out in hospitals throughout China. After the 5th edition of American Guidelines for Neonatal Resuscitation was published in the end of 2005 and in 2006,[8,9] its Chinese version was also published in 2006.[10] The new guidelines were not changed much compared with the 2000 edition, on which the Chinese guidelines were largely based.[11] In this article, we introduce the 4th edition of Chinese Guidelines for Neonatal Resuscitation of Asphyxia, and also discuss the modification of neonatal resuscitation techniques compared to the previous edition.[3]
The new neonatal flow algorithm (Fig. 1)
There are 21 frames in the old flow algorithm.[3] In contrast, the new flow algorithm has a simple vertical drop down direction, including 2 evaluation frames and 4 action frames which represent four resuscitation steps (A, B, C and D), respectively. In addition, the 3 care frames are included but not considered as part of the resuscitation process. Consequently, the new flow algorithm has only 6 main frames containing information. So it is easy for training.
The new flow algorithm demonstrates the speed for each step. Approximately 30 seconds is allotted to complete each step of A, B and C, then reevaluate or decide whether to progress to the next step. Immediately after birth, a rapid evaluation of 4 characteristics (gestation, meconium, breathing, muscle tone) needs only several seconds (usually no more than 5 seconds). Later evaluations (including heart rate, respiration) during resuscitation need another short time. So the decision of whether or not to initiate resuscitation is made using the above rapid evaluation rather than Apgar scores given at 1 minute after birth. Apgar scores are only used to evaluate the whole birth condition and resuscitation effects of the newborn.
The arrows in the flow algorithm show clearly what the sequence of resuscitation procedure is: A (airway), i.e., clearing the airway or endotracheal intubation (ET) when indicated; B (breathing), i.e., establishing breaths with bag and mask or bag and endotracheal tube to provide positive pressure ventilation; C (circulation), i.e., promoting circulation by chest compressions which are likely to compete with effective ventilation; and D (drug). The most common mistake is delivering chest compressions and/or drugs before insuring adequate ventilation. These steps may lead to ineffective resuscitation if ineffective ventilation is performed. It should be said that no chest compressions are necessary if ET is not needed, and no drug is necessary if chest compressions are not needed.
The likelihood of progressing to the next in the flow algorithm is decreased progressively just as in a reversed pyramid (Fig. 2). The top line of evaluation steps should be done in all newborns, and the below steps are gradually tapered. Approximately 10% of newborns require some ventilation assistance to begin breathing at birth, and approximately <1% of newborns require chest compressions or drugs. We have reported resuscitation in 8101 cases, including step A 8101 cases (100%), step B 963 cases (11.9%), steps C 59 cases (0.7%) and step D 14 cases (0.17%). The case fatality rate is merely 0.4%.[12] In other countries,[13] only 0.12% of 30 839 cases were given chest compressions and/or drugs. It should be emphasized that the most important step or the key procedure in neonatal resuscitation is ventilation. Care givers should review their resuscitation techniques if chest compression and/or drugs have been administered frequently during a period of time.
Fig. 1. New flow algorithm for neonatal resuscitation (from AAP 2006[9]) (*: Endotracheal intubation may be considered at several steps).
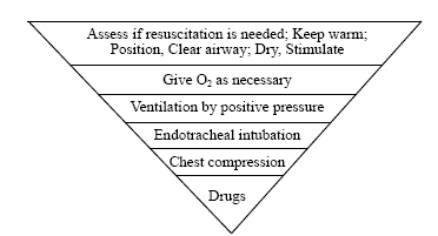
Fig. 2. Reversed pyramid of resuscitation (from AAP 2006[10]).
There are arrows progressing back up the new flow algorithm when resuscitation becomes effective (from frame D to C, or from C to B). These measures taken to avoid excessive resuscitation have not been emphasized in the past editions of Guidelines for Neonatal Resuscitation of Asphyxia.
The new flow algorithm points out clearly that different grades of resuscitation (mild, moderate or heavy) should have different levels of care after resuscitation. Following resuscitation, once adequate ventilation and circulation have been established, the infant should be maintained in or transferred to an environment in which close monitoring and care can be provided. The above feature has also not been reflected in the former flow algorithm.
Major technical improvement of resuscitation in the new guidelines
Newly born infants can generally be identified by a rapid assessment of the following 4 characteristics before initial resuscitation in several seconds: Term gestation? Amniotic fluid clear? Breathing or crying? Good muscle tone? This embodies the EDA-cycle principle (first E, evaluation, then D, decision, then A, action), which is emphasized differently in the current edition of the guidelines by evaluation first rather than initial resuscitation first.
The new guidelines are added with an additional algorithm if the amniotic fluid contains meconium, which describes clearing of the meconium (Fig. 3) and suctioning of the trachea (Fig. 4).
*: "vigorous" is defined as strong respiratory efforts, good muscle tone, and a heart rate greater than 100 bpm.
Fig. 3. Additional small flow algorithm for meconium clearing (adapted from AAP 2006[9]).
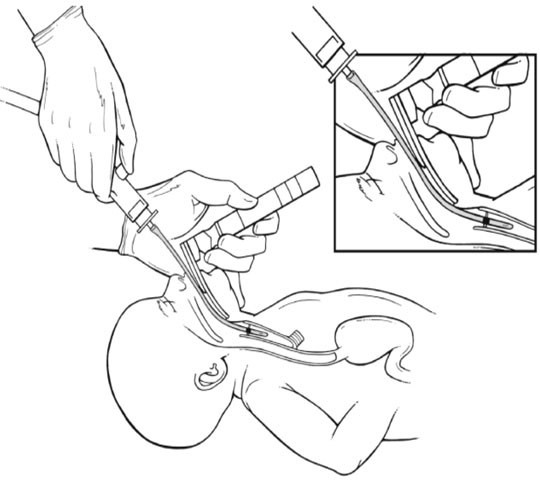 Visualizing the glottis and suctioning meconium from the trachea using a laryngoscope and endotracheal tube. Visualizing the glottis and suctioning meconium from the trachea using a laryngoscope and endotracheal tube.
Fig. 4. Meconium suction by the endotracheal tube method (adapted from AAP [5]).
Current recommendations no longer advise routine intrapartum oropharyngeal and nasopharyngeal suctioning for infants born to mothers with meconium staining of amniotic fluid. When the amniotic fluid is meconium-stained, infants should be endotracheally intubated immediately and suctioned only if they are not vigorous. A vigorous infant is defined as one who has strong respiratory efforts, good muscle tone, and a heart rate >100 beats per minute (bpm). Tracheal suctioning is not necessary for babies with meconium-stained fluid who are vigorous. In the previous editions, endotracheal suctioning is based on whether the meconium is thin or thick.
The meconium suction catheter is a disposable plastic tube used specifically for suctioning meconium. One end of the meconium suction catheter should be connected to an endotracheal tube and the other to the suction apparatus. Suction pressure should not exceed 100-200 mmHg. Tracheal suctioning would be accomplished by applying suction directly to a tracheal tube as it is withdrawn from the airway. Intubation and suction can be repeated once until little additional meconium is recovered (Fig. 4) but only if the heart rate remains stable. Suction of meconium from the trachea by passing a suction catheter through an endotracheal tube as recommended previously should be avoided and the size of the suction catheter is too small to be effective.
A large-hole suction catheter (12F to 14F recom-mended now rather than 10F in the previous edition) can be used for suctioning secretions, amniotic fluid and meconium in the nose, mouth, and posterior pharynx. This allows rapid, sufficient, and safe suctioning.
The newly born infant should be placed in a supine position with the head slightly extended in a "sniffing" position to open the airway. If respiratory effort does not produce effective tidal ventilation, often the airway is obstructed and immediate efforts must be made to correct overextension or flexion of the neck or to remove secretions. A blanket or towel placed under the shoulder may be helpful in maintaining proper head position.
In the former edition, the infants were dried before suctioning in the initial steps. In the new guidelines, if suctioning is necessary, clear secretions first and then dry the baby. Drying before the secretions have been wiped off produces enough stimulation to initiate effective respirations in most infants and the secretions in the nose and mouth may be aspirated.
The concept of chest massage is incorrect and is no longer used. It is called chest compression in the new guidelines.
At present, the indication for chest compression is a heart rate <60 bpm despite adequate ventilation with 100% oxygen for 30 seconds. Although it is a common practice to give compression if the heart rate is around 60 to 80 bpm, this has been changed to remain simple.
Reassessment of the heart rate is made for approximately every 30 seconds, and chest compression is continued until the appearance of a spontaneous heart rate of ¡Ý60 bpm. Thus, two indications are known by remembering 60 bpm, and it is effective and easy for training.
Compression is delivered 1-2 cm in the old edition, but it is impossible to measure without reference. In the new edition, compressions should be delivered approximately one third of the anterior-posterior diameter of the chest (about 5-6 cm for term babies) to generate a palpable pulse. This makes the guidelines easier to understand and follow than before.
Compression position is defined as the lower third of the sternum in the new guidelines rather than the boundary location of middle third and lower third of the sternum or 2 cm under the nipple line in the sternum as described before. The new description is more acceptable and applicable for rapid resuscitating actions.
The compression rate is 120 bpm in the old edition, and now has been changed to 90 bpm in the new guidelines. This helps to prevent hypoventilation. There still should be a 3:1 ratio of compressions to ventilation, i.e., 3 compressions with 1 breathing to achieve approximately 120 events per minute. Coordination of compressions and ventilations to avoid simultaneous delivery will prevent hypoventilation.
The assisted ventilation rate should usually be 40 to 60 breaths per minute without chest compression, but would be decreased to 30 breaths per minute during chest compressions rather than 40 breaths per minute in the old edition.
There are five indications for ET during neonatal resuscitation in the old edition: (1) when tracheal suctioning of meconium is required; (2) if positive pressure ventilation is prolonged; (3) if bag-mask ventilation is ineffective; (4) when tracheal administration of medications is desired; and (5) special resuscitation circumstances, such as congenital diaphragmatic hernia or use of surfactant for extremely low-birth weight infants. The new edition is added with a new indication and puts it at the third position in the list of indications: when chest compression is performed because chest compression may diminish the effectiveness of ventilation. Remember not to initiate the compression until full lung inflation and ventilation have been established.
The key point of successful ET is putting blade tip of a laryngoscope into the epiglottis vallecula (Fig. 5) rather than pressing the epiglottis with a blade as described previously (Fig. 6)[14], then lifting the blade gently with downward pressure on the cricoid, which may help bring glottis into view, and inserting the tube to an appropriate depth through the vocal cords. The new method is easy to learn in training and its success rate for intubation is much higher.
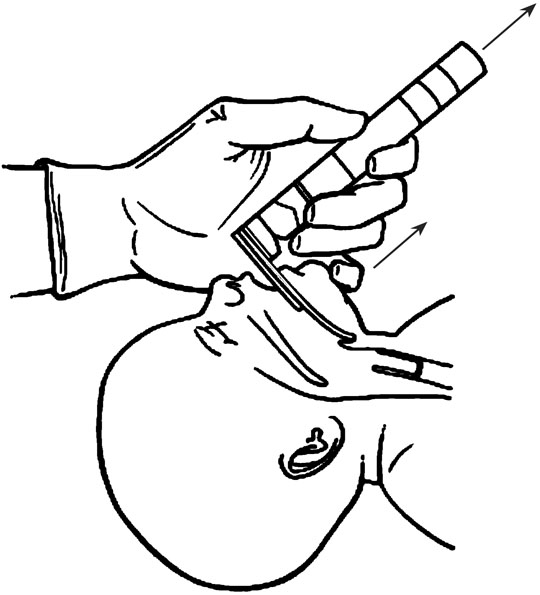 
Fig. 5. The new ET method: putting blade in the epiglottis vallecula and lifting (adapted from AAP[5]). Fig. 6. The old ET method: pressing epiglottis with a blade (adapted from Zhou et al[14]).
Drugs are rarely indicated in resuscitation of the newly born infants (only 1¡ë-5¡ë). When medications are given immediately despite adequate ventilation with 100% oxygen and chest compression, the heart rate remains 60 bpm. There are 3 commonly used drugs during resuscitation in the newborn: epinephrine, bicarbonate and volume expanders in the new edition rather than 5 drugs in the old one. The 2 drugs not listed in new edition are dopamine and naloxone hydrochloride.
Dopamine is usually used postresuscitation in neonatal intensive care units. Naloxone hydrochloride is a narcotic antagonist. It is specifically indicated for reversal of respiratory depression in a newly born infant whose mother received narcotics within 4 hours of delivery. It is always necessary to establish and maintain adequate ventilation and circulation before administration of naloxone. Calcium gluconate or atropine might be considered under very special circumstances.
Volume expansion is considered when there is suspected blood loss or the infant appears to be in shock (pale, poor perfusion, weak pulse) and has not responded adequately to other resuscitative measures. The fluid of choice for volume expansion is an isotonic crystalloid solution such as normal saline or Ringer's lactate rather than whole blood or albumin-containing solutions as before. Administration of whole blood or albumin-containing solutions are limitedly and rarely available during resuscitation. The initial dose of volume expander is 10 ml/kg, which is given by slow intravenous push over 5 to 10 minutes. Normal saline or Ringer's lactate solution can improve the blood capacity and tissue perfusion rapidly so as to increase the opportunity of survival. When resuscitating premature infants, care should be taken to avoid giving volume expander too rapidly, because rapid infusion of large volume has been associated with intraventricular hemorrhage.
Funding: None.
Ethical approval: Not needed.
Competing interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributors: ZXY wrote the first draft of this paper. ZQS analyzed the data.
References
1 Shi SZ. Suggestion about the rescue methods of neonatal asphyxia. Chin J Pediatr 1965;14:136-137.
2 Ji XC, Shi SZ, Hu HF, Yu RJ, Shao XM, Xu FL. Suggestion about the methods of neonatal resuscitation on asphyxia. Chin J Pediatr 1983;21:299-301.
3 Shi SZ. Suggestion about the methods of neonatal resuscitation on asphyxia. Chin J Pediatr 1994;32:301-302.
4 Ye HM. Conference summary of the expert committee on neonatal resuscitation program. Chin J Perinatal Med 2004;7:171-172.
5 American Academy of Pediatrics (AAP), American Heart Association (AHA). Neonatal resuscitation on asphyxia (Chinese edition, Beijing). Cooperation program of Department of Maternal and Child Health Care and Community Health, Health Ministry of China, 2004.
6 Yu RJ, Ye HM, Huang XH, Wang DH. Guidelines of neonatal resuscitation on asphyxia. Chin J Pediatr 2005;43:381-384.
7 Yu RJ, Ye HM, Wang DH. Program of neonatal resuscitation on asphyxia: the major changes between the old and new editions. Chin J Pediatr 2005;43:385.
8 2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: part13: Neonatal resuscitation guidelines. Circulation 2005;112(24 suppl):IV-188-IV-195.
9 American Heart Association, American Academy of Pediatrics. 2005 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC) of Pediatric and Neonatal Patients: Neonatal Resuscitation Guidelines. Pediatrics 2006;117:e1029-e1038.
10 Department of Maternal and Child Health Care and Community Health, Health Ministry of China (translated & edited by Ye HM, Yu RJ). Textbook of neonatal resuscitation on asphyxia (Chinese version from 5th American textbook of neonatal resuscitation). Shanghai: Press of the Second Military Medical University, 2006.
11 AHA/AAP Neonatal Resusciation Program Steering Committee. Textbook of neonatal resuscitation, 4th ed. Elk Grove Village: American Academy of Pediatrics, 2000.
12 Zeng SP, Zhu, XY, Fang HQ, Hou ZX, Liu G, Lin HL, et al. Research and effect of neonatal resuscitation in high risk newborns. Chin J Perinatol Med 1998;1:64.
13 Ginsberg HG, Goldsmith JP. Controversies in neonatal resuscitation. Clin Perinatol 1998;25:1-15.
14 Zhou XG, Xiao X, Nong SH. Therapeutics for neonatal mechanical ventilation. Beijing: People Health Press, 2004: 435-454.
Received December 26, 2006; Accepted after revision March 12, 2007
|

