|
Successful separation of ischiopagus tetrapus
conjoined twins
Xi-Sheng Zhang, Zhi-Gang Feng, Qi-Xin Xiong, Min-Ju Li, Da-Xing Tang
Hangzhou, China
Author Affiliations: Department of Pediatric Surgery, Children's Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Zhang XS, Feng ZG, Xiong QX, Li MJ, Tang DX)
Corresponding Author: Xi-Sheng Zhang, MD, Department of Pediatric Surgery, Children's Hospital, Zhejiang University School of Medicine, Hangzhou 310003, China (Tel: 86-571-87061007 ext 60511; Fax: 86-571-87084307; Email: dreamsky_198@hotmail.com)
Background: A pair of female ischiopagus tetrapus conjoined twins were transferred to our hospital when they were 3 days old and with a total weight of 3850 g. They were fused face to face from the umbilicus to the pelvis at an angle of 60 degrees. There was a single umbilicus ventrally. The twins shared an anus, and each infant exhibited a urethral and two vaginal orifices.
Methods: A series of radiological examinations showed two separate normal upper tracts, two small intestines joined at the common terminal ileum, a single cecum, and a common colon connected with an anus in twin A. They had two retropubic bladders close together as a large bladder with a very thin midst membrane, two sacrums faced each other and division of pubic symphysis. Separation surgery was performed on the twins at the age of 3 months.
Results: The surgery lasted for 4.5 hours. Both infants were transferred to the Neonatal Intensive Care Unit (NICU) after the operation. Twin A died 6 hours after the operation for unknown reasons. Twin B survived and the follow up showed that she became a normal and healthy girl.
Conclusions: Ischiopagus conjoined twins are rare and their separation is more difficult for the variable anatomy. Careful preoperative evaluation and planning are very important. The connecting bridge should be enlarged sufficiently before operation so as to repair the abdominal wall.
Key words: conjoined twins; ischiopagus; tetrapus; separation; surgery
World J Pediatr 2007;3(3):228-231
Introduction
Conjoined twinning is a rare occurrence, its incidence is estimated to be around 1 in 250 000 live births. The ischiopagus variety is rarer. In case of its rarity and variable anatomy, no definite treatment plan can be adapted.
Since the initial case reported by Eades et al in 1966,[1] few cases of separation of ischiopagus tetrapus conjoined twins were reported around the world and only one case in China.
We present here the management of a pair of female ischiopagus tetrapus conjoined twins at the Department of Surgery in Children's Hospital, Zhejiang University School of Medicine, China. Preoperative evaluation, surgical planning and postoperative treatment were reported.
Case report
A pair of female ischiopagus twins were born in Rui'an, Zhejiang Province, China in May 2000, to a 23-year-old gravida 1, para 1 mother. The pregnancy and delivery were uneventful.
The conjoined twins were referred to our hospital when they were 3 days old. They had a total weight of 3850 g and were fused face to face at the lower abdomen and the pelvis at an angle of 60 degrees (Fig. 1). Each twin was normal and separated from 1 cm up the umbilicus above the fused area. Each twin had her own lower limbs. The circumference of union was 34 cm and there was a single umbilicus ventrally and a pair of vulvas dorsolaterally.
X-ray showed a single pelvic ring, two sacrums faced each other, and a division of symphysis pubes. Upper and lower contrast studies demonstrated two separate normal upper gastrointestinal tracts. Two small intestines joined at the common terminal ileum about 12 cm long and a single cecum, then they entered the common colon connected with an anus in twin A (Fig. 2). Contrast studies revealed four normal kidneys and two retropubic bladders. But the bladders were so close together as a large bladder with a very thin midst membrane (Fig. 3). Twin A had a perineal orifice, an anus, a vagina and a urethral opening. Twin B had a urogenital sinus with an imperforate anus and duplicated vaginas, each with a separate uterus. MRI showed a common colon led to twin A. Twin B had an imperforate anus (Fig. 4-6). Doppler echocardiography confirmed that twin A had a patent foramen ovale and twin B had an atrial septal defect.
Because the twins were weak, their weight was only 3850 g and twin B was easy to suffer from respiratory tract infection. The separation was delayed tentatively, and they were transferred to the Intensive Care Unit (ICU). They were both fed with high-calorie diet and subjected to treatment of jaundice, diarrhea, omphalitis and bronchitis. Instead of using tissue expanders, the angle of body bridge between the two twins enlarged when they were washed every day. With the angle was enlarged from 60 degrees to 180 degrees, the skin of the body bridge was sufficient for repairing the defect of the abdominal wall. The separation was performed on the twins 3 months later with a body weight of 7.2 kg. A series of examinations were performed on the twins including cystography, vaginoscopy, CT, MRI and Doppler echocardiography before the operation.
A circumferential incision was made in the connecting bridge. Exploration of the abdomen confirmed the preoperative diagnosis. The small intestines of the twins ended in a common ileum (about 12 cm long) and a single cecum. There were two appendices which connected the cecum. A single distended colon led to an anus in twin A. The shared intestines received a dual mesentery blood supply from the twins. The distant ileum of twin A near the common ileum had a Meckel's diverticulum. The large bladder was separated into two halves by a very thin membrane (just like a piece of paper). On the top, there was a fine fibrous cord. Each "half" of the bladder had two ureters from two kidneys, and looked normal. Twin B had two uteruses, four ovaries and uterine tubes.
After a study of the colonic blood supply, we decided that the proximal half of the common colon in continuity with the ileum was given to twin B and the distal half to twin A. The small bowel of twin A was divided at the level of the Meckel's diverticulum and an ileocolostomy was established in twin A. Twin B received an ileostomy, while the two appendices were resected (Fig. 6). In order to facilitate closure and pelvic stabilization, iliac osteotomies were performed on the twins. Fascial and skin closure of the abdomen was done easily on the twins without any tension. The procedure lasted for 4.5 hours and 50 ml blood was lost. Both infants were transferred to the ICU after operation. Unfortunately, twin A died from unknown reasons 6 hours after operation. Twin B did well postoperatively and was discharged at 4 months of age. She subsequently was re-admitted for colonstomy revision and reconstruction of imperforate anus after one year. A 3-year follow-up showed that she was an active intelligent child.
 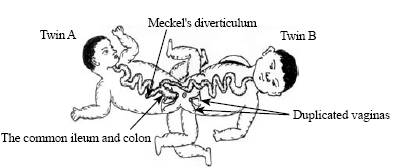
Fig. 1 Fig. 2
Fig. 1. Ischiopagus tetrapus conjoined twins. Fig. 2. Preoperative view of the twinning.
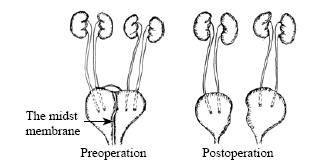 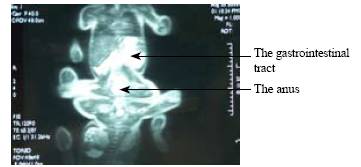
Fig. 3 Fig. 4
Fig. 3. Separation planning on the two bladders.Fig. 4. The gastrointestinal contrast study of twin A.
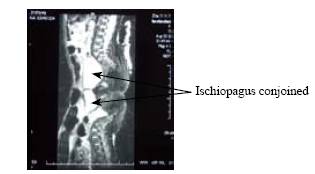 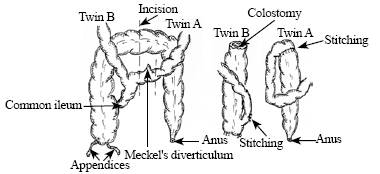
Fig. 5 Fig.6
Fig. 5. MRI view of the ischiopagus conjoined twins. Fig. 6. Common ileum and colon.
Discussion
Conjoined twins are most challenging patients faced by pediatric surgeons because of their rarity, variable anatomy, and no definite treatment. Symmetrically conjoined twins are rarely seen, about 1 in 50 000 births. In China, the incidence rate is 0.3/10 000.[2] Only 6% of conjoined twins are of ischiopagus type in which the twins are joined symmetrically at the pelvis and fusion begins at the level of the common umbilicus. So far, only 20 cases have been reported.[3] Coupling of the gastrointestinal tract occurs at a Meckel's diverticulum, distal small and large intestines usually become a common tract and have a dual blood supply. The upper urinary tract is most commonly duplicated. Tetrapus is a subtype in which all 4 lower extremities are present and oriented at right angles to the axis of the common trunk. The twins in our study had a Meckel's diverticulum, single distal small and large intestines, imperforate anus, urogenital sinus, duplicated vaginas and uteruses, and "fusion" of two bladders. There were two vaginal orifices, an urethral orifice and an anal fovea in twin B's cloaca. Careful preoperative planning is very important to achieve excellent outcomes.[4] Plain films, vaginograms, intravenous pyelograms, barium enema, and upper gastrointestinal series, ultrasonography, echocardiography, CT, and MRI were performed. Advanced imaging techniques are amazingly efficient in depicting complex fusions that have to be accurately recognized when planning separation strategies.[5] So the correct diagnosis and detailed planning can be done successfully.
The timing of separation is based on adequate preoperative studies and sufficient preparations for abdominoperineal closure. The time of operation and the mode of treatment have to be tailored according to the local circumstances and organ sharing in each individual pair.[3-6] O'Neill et al[7] found that a survival rate of 50% can be reached when separation was done in the neonatal period while a survival rate of 90% when separation occurred beyond 4 months of age. But others[8] considered that the death was not related to the age at separation. There were three indications for emergency separation: (1) when serious illness in one twin threatens the life of the other; (2) the presence of a surgically correctable life-threatening anomaly; (3) when a traumatic injury occurs to the connecting bridges of tissue or viscera.[9] We did this separation when the twins were 3 months old, because they were easy to suffer from infection of the bronchi or lung despite they had been in the ICU. Thus we had to advance the time of the operation, which may be one of the causes of the death of twin A. The troubles of the respiratory and circulation systems may be another important cause of the Twin A's death. But the real cause is unknown because their parents did not agree to do autopsy.
For increased abdominal wall coverage, many ischiopagus conjoined twins had to be used intraperitoneal tissue expander or pneumoperitoneum before separation surgery. Reports on the tissue expander usage in children showed a complication rate of 26%, and infections are the most common reason for expander removal.[10] We observed that the connecting bridge of our ischiopagus conjoined twins could be enlarged by extending. When our nurses cleaned these conjoined twins every day, they gradually enlarged the bridge angle between them from 60 degrees to 180 degrees by letting the twins lying flat on the back. After 3 months, the skin of the bridge was enough for repairing the defect of the abdominal wall for separation.
Ischiopagus conjoined twins manifest an interesting array of spinal abnormalities, which present challenges, not only at the time of separation, but also in their long-term management.[11] The deformity in the ischiopagus tetrapus pelvis is purely an external rotation of the posterior segment. Posterior iliac osteotomy alone is therefore able to restore pelvic symmetry and prevent rediastasis of the symphysis pubis.[12]
In conclusion, detailed systemic investigation, tailored preoperative plannig and advanced coordinated teamwork are very important for the separation of the conjoined twins.
Funding: None.
Ethical approval: Not needed.
Competing interest: None declared.
Contributors: ZXS proposed the study and wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts.
References
1 Eades JW, Thomas CG. Successful separation of ischiopagus tetrapus conjioned twins. Ann Surg 1996;164:1059-1072.
2 Liang J, Xu CL, Wang Y. Epidemiological survey of conjoined twins in China. JWCUMS 1999;30:56-58.
3 Qazi AQ, Haq AU, Burki T, Khan A, Mansoor K, Chaudhry A, et al. Separation of xiphi-omphalo-ischiopagus tetrapus twins with favorable internal anatomy. J Pediatr Surg 2002;37:E9.
4 Kim SS, Waldhausen JH, Weidner BC, Grady R, Mitchell M, Sawin R, et al. Perineal reconstruction of female conjoined twins. J Pediatr Surg 2002;37:1740-1743.
5 Martinez L, Fernandez J, Pastor I, Garcia-Guereta L, Lassaletta L, Tovar JA. The contribution of modern imaging to planning separation strategies in conjoined twins. Eur J Pediatr Surg 2003;13:120-124.
6 Yang TH, Li J, Huang XB, Zuo GH, Luo YS, Xiao YB, et al. Diagnosis and treatment of conjoined twins a report of two cases. Chin J Pediatr Surg 2002;23:445-447.
7 O'Neill JA, Holcomb GW, Schnaufer L, Templeton JM, Bishop HC, Ross AJ, et al. Surgical experience with thirteen conjoined twins. Ann Surg 1988;208:299-312.
8 Doski JJ, Heiman HS, Solenrger RI, Stefko RM, Kuivila T, Rozanski TA, et al. Successful separation of ischiopagus tripus conjoined twins with comparative analysis of methods for abdominal wall closure and use of the tripus limb. J Pediatr Surg 1997;32:1761-1766.
9 Filler RM. Conjoined twins and their separation. Semin Perinatol 1986;10:82-91.
10 Iconomou TG , Michelow BJ , Zuker RM. Tissue expansion in the pediatric patient. Ann Plast Surg 1993;31:134 -140.
11 Fieggen AG, Dunn RN, Pitcher RD, Millar AJ, Rode H, Peter JC, et al. Ischiopagus and pygopagus conjoined twins: neurosurgical considerations. Childs Nerv Syst 2004;20: 640-651.
12 Verrier MD, Hastings CJ, Hoffman EB. Posterior iliac osteotomy in ischiopagus tetrapus twins. J Pediatr Orthop 2000;20:807-811.
Received January 8, 2007 Accepted after revision April 27, 2007
|

